To ease burdens on the health system, reduce inefficiencies and improve quality of patient care, innovative methods of delivering effective healthcare must be developed. Remote patient monitoring, which refers to the measurement and analysis of a patient’s health status without them needing to be physically present in a traditional healthcare setting or in the presence of a health professional, is emerging as a promising way to address Australia’s growing healthcare pressures.
In this webinar, our panel will discuss:
– The trends driving remote patient monitoring and how these systems are utilising wearable technology;
– Lessons learned from initial remote patient monitoring rollouts, the key challenges faced and how these were addressed;
– The costs and benefits of remote patient monitoring, and the pros and cons for patients and clinicians;
– How to identify and engage patients for remote monitoring and the factors that make some individuals poor candidates for this model of care;
– Clinical results from remote patient monitoring programs;
– Key workflow and set-up considerations, and ongoing systems, processes and governance;
– Issues related to patient privacy, information security, interoperability, data sharing and supplying equipment versus patients using their own devices; and
– Gains made during COVID-19, untapped opportunities and the future outlook.
Please join us for what promises to be an insightful and informative conversation.
This webinar is proudly brought to you by DHCRC, Curtin University and La Trobe University.
Panelist bios
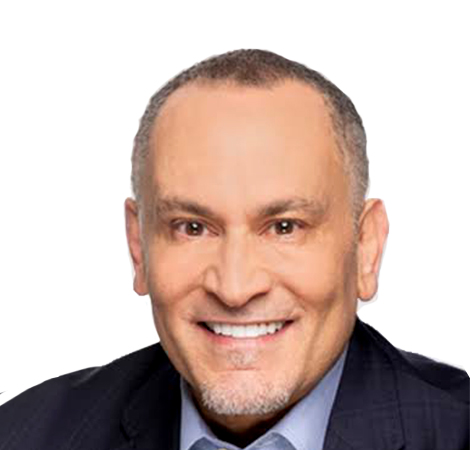
Dr Neale Fong (panel chair), Western Australian Country Health Service Board Chair
 Neale is a registered medical practitioner with over 30 years’ experience in medical and health care delivery and a wide range of leadership roles. His strengths lie in systems management, reform and change management, developing strategic directions and leading and managing both health policy and operational entities. He has held and continues to hold very senior positions in all health care sectors covering government services, private hospitals, academia, health research, public health, aged care and not for profit organisations. Neale is currently Chair of the Western Australian Country Health Service Board, Professor of Healthcare Leadership at Curtin University, Chairman of Bethesda Health Care, National President of the Australasian College of Health Service Management, a Director on the Digital Health CRC Board and was Project Lead to the Australian Health Ministers Council in developing Australia’s first Health Leadership Development Capability Framework.
Neale is a registered medical practitioner with over 30 years’ experience in medical and health care delivery and a wide range of leadership roles. His strengths lie in systems management, reform and change management, developing strategic directions and leading and managing both health policy and operational entities. He has held and continues to hold very senior positions in all health care sectors covering government services, private hospitals, academia, health research, public health, aged care and not for profit organisations. Neale is currently Chair of the Western Australian Country Health Service Board, Professor of Healthcare Leadership at Curtin University, Chairman of Bethesda Health Care, National President of the Australasian College of Health Service Management, a Director on the Digital Health CRC Board and was Project Lead to the Australian Health Ministers Council in developing Australia’s first Health Leadership Development Capability Framework.
Dr Louise Tulloh, President of the Australasian College of Sport and Exercise Physicians

Louise is the President of the Australasian College of Sport and Exercise Physicians. She practises at North Sydney Sports Medicine Centre and is a co-founder of myscoreit, a health tech start-up to measure patient reported outcome measures in musculoskeletal care.
Her clinical interests include persistent pain, issues facing women athletes and utilising a holistic, biopsychosocial model of care.
Dr Liliana Laranjo, MD, MPH, PhD, Research Fellow, Westmead Applied Research Centre, The University of Sydney
 Liliana Laranjo is a Medical Doctor (General Practitioner) with a Master of Public Health from Harvard University, and a PhD in Digital Health. She is working as a Research Fellow in Digital Health at the Westmead Applied Research Centre, Faculty of Medicine and Health, University of Sydney. Her current research focuses on the use of digital health (smartphone applications, text messages, wearable and wireless devices) to promote behaviour change, patient-centred care, and primary and secondary prevention of chronic conditions.
Liliana Laranjo is a Medical Doctor (General Practitioner) with a Master of Public Health from Harvard University, and a PhD in Digital Health. She is working as a Research Fellow in Digital Health at the Westmead Applied Research Centre, Faculty of Medicine and Health, University of Sydney. Her current research focuses on the use of digital health (smartphone applications, text messages, wearable and wireless devices) to promote behaviour change, patient-centred care, and primary and secondary prevention of chronic conditions.
Andre Ferretto, Founder and Managing Director, HalleyAssist® Pty Ltd
 Andre believes that businesses should have a clear purpose and contribute to society. This belief, combined with a passion for emerging technology led him to found HalleyAssist®. This came about after an ageing related health issue affected his own family. Andre found a lack of usable assistive technology that worked for his family, so he developed his own. HalleyAssist® technology consists of a novel AI powered, IOT in-home health monitoring technology. Andre has authored a number of peer reviewed publications on the novel AI system. This system analyses the sensor data to learn normal movements and behaviours of the monitored individual. It delivers information to carers on the individual’s movements and status in real time and will alert carers to urgent health issues such as falls and longer-term changes in physical activity, hydration and potential infections. This information delivery allows earlier intervention to provide better health outcomes and lower healthcare costs.
Andre believes that businesses should have a clear purpose and contribute to society. This belief, combined with a passion for emerging technology led him to found HalleyAssist®. This came about after an ageing related health issue affected his own family. Andre found a lack of usable assistive technology that worked for his family, so he developed his own. HalleyAssist® technology consists of a novel AI powered, IOT in-home health monitoring technology. Andre has authored a number of peer reviewed publications on the novel AI system. This system analyses the sensor data to learn normal movements and behaviours of the monitored individual. It delivers information to carers on the individual’s movements and status in real time and will alert carers to urgent health issues such as falls and longer-term changes in physical activity, hydration and potential infections. This information delivery allows earlier intervention to provide better health outcomes and lower healthcare costs.
Jo Stevens, Manager Chronic and Complex Care, Barwon Health, Victoria (BN Hon, BA, BCom, Cert Rehab Nurse, Grad Cert Clinical Redesign)
 Jo has been working in various leadership roles within Barwon Health for over 25 years.
Jo has been working in various leadership roles within Barwon Health for over 25 years.
In 2014 Jo commenced the implementation of the tele-health intervention Personalised Health Care that aims to enhance the health literacy and self-management of patients living with chronic disease.
Jo is responsible for the implementation of the Department of Health and Human Services Healthlinks pilot which aims to better manage those clients in our community that are at significant risk of hospitalisation.