hidden
hidden text
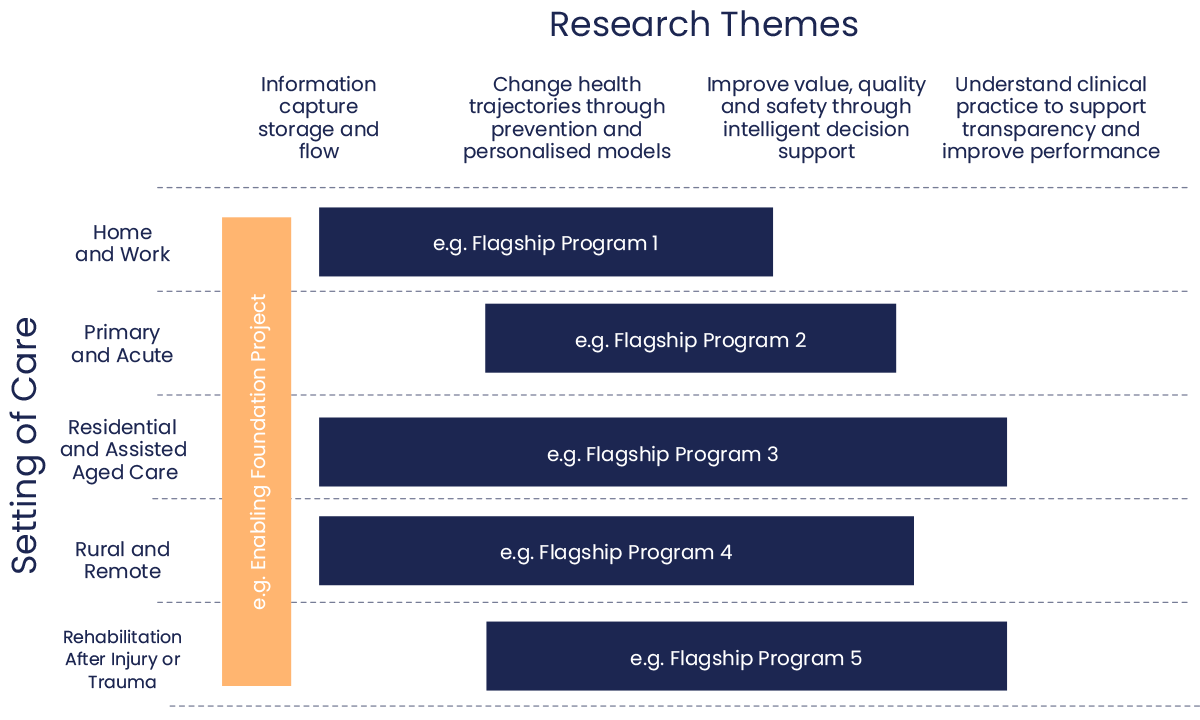
Research and Development Matrix
hidden
hidden
This is a hidden content
Flagship Programs
A health ecosystem Flagship Program is made up of several linked projects. Flagship Programs are the direct output of a codesign process of iterative development with multi-stakeholder reference groups and our research team. They focus on areas of demonstrated industry need within the health system for a targeted and collaborative program of work supported by data and digital technology. Flagship Programs provide a framework for the development of substantial linked projects and will often extend across cells in the Research and Development Matrix.
From the outputs of the workshops and from ongoing consultation, an initial seven Flagship Programs have been developed. Four of these are cross-cutting and three are of special interest and relate to specific settings of care.
To maximise return on investment and impact we will look to develop multi-participant projects spanning our Flagship Programs where possible. However, our intention is to commence with a series of smaller projects that will link up to form the foundation for our Flagship Programs.
| Settings of Care | Flagship | Summary |
|---|---|---|
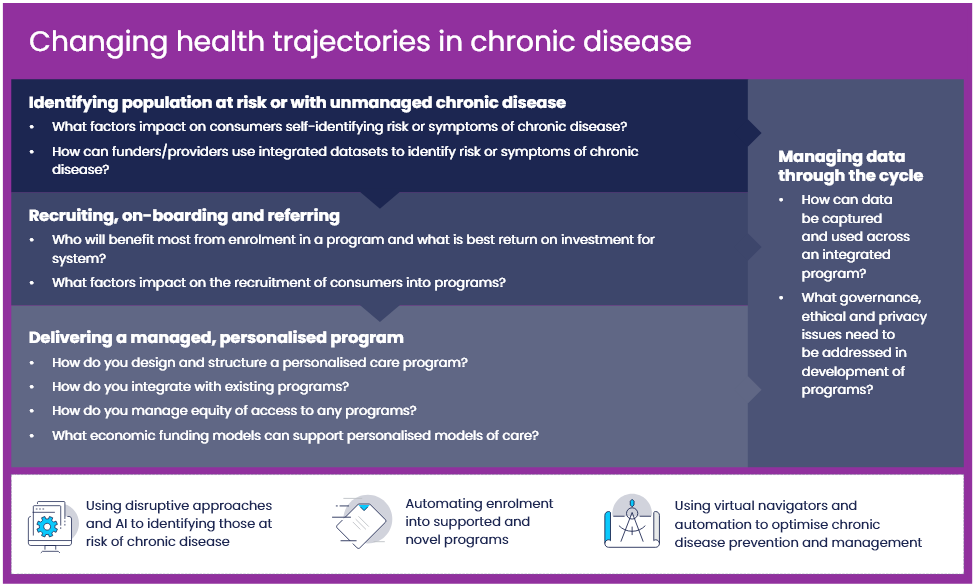
| Common across all Settings of Care | Changing health trajectories in chronic disease | Use different data sets to identify populations who have or are at risk of developing chronic disease. Provide personalised models of care, digitally- supported behavioural interventions and end-to-end management. Avoid unnecessary hospital admissions and empower people to manage their own health and wellness. |
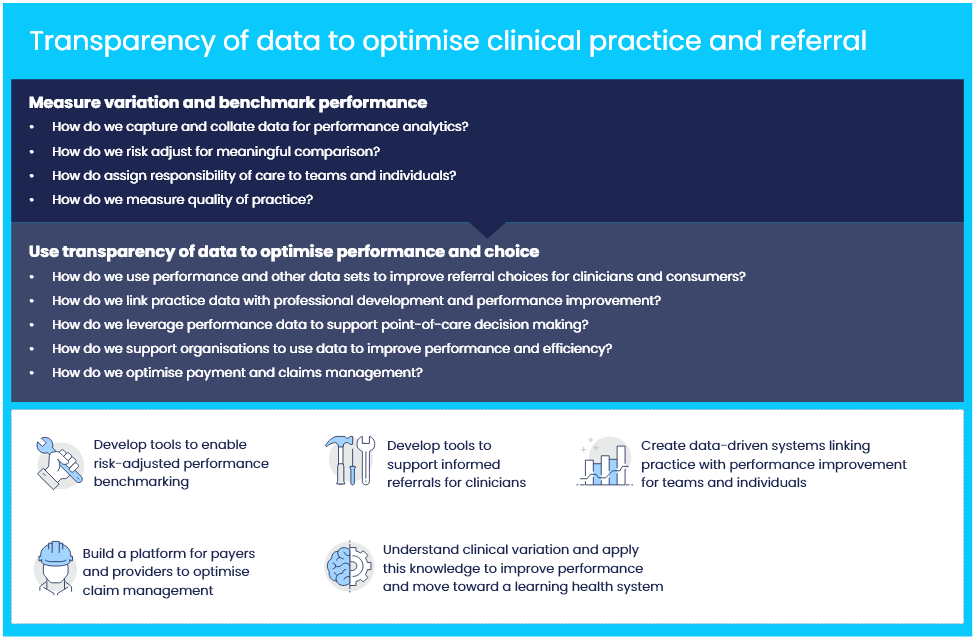
| Transparency of data to optimise clinical practice and referral | Use health care, administrative and other data to measure and understand clinical variation and practice; support reflection andpersonalised professional development; support appropriate consumer referral; and drive efficiency through payment and claims optimisation. |
|
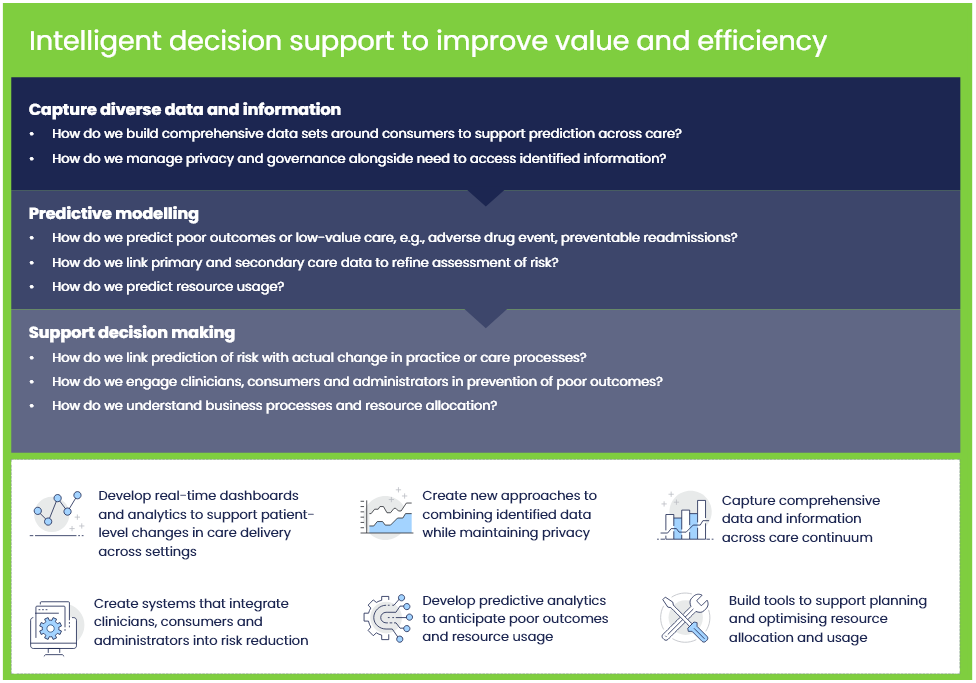
| Intelligent decision support to improve value and efficiency | Use comprehensive data and information across care continuum tounderstand consumer risk and organisational performance. Provide intelligence to consumers, clinicians, managers and administrators to predict and prevent poor outcomes and low-value care. E.g., improve quality use of medications. Support resource allocation and business efficiency. |
|
| Enabling information discovery and application | Explore issues surrounding ethics, governance and privacy of linking and using health data. Development of targeted tools resources to support and facilitate health data sharing and application in practice, quality improvement, trials and research. |
|
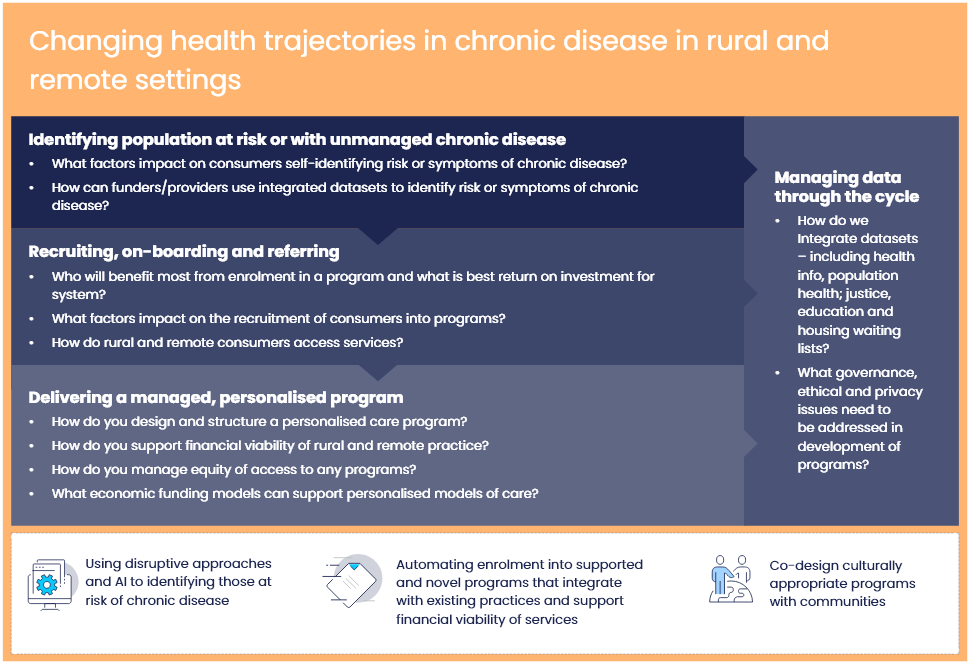
| Rural & Remote | Changing health trajectories in chronic disease in rural and remote settings | Address issues that are specific to rural and remote including access, maintaining viable healthcare services, integrating social determinants of health, overcoming technology challenges, reducing digital divide and co-designing culturally appropriate programs. |
| Rehabilitation following injury or trauma | Digitally coordinated and supported rehabilitation management | Use comprehensive data following injury and link with previous history to predict risk and improve outcomes of rehabilitation. Deliver personalised, technology-supported interventions with portals that support communication between care providers and with clients and family |
| Residential and Assisted Aged Care | Digitally supported and coordinated aged care management | Use resident, service and clinical data to improve quality, reporting and business efficiency. Support coordinated, shared care and resident quality of life through personal and family portals. Provide real-time dashboards and knowledge to support continuous quality improvement and decision support. |